Mandibular defects include only bony defects of the mandible after surgical excision of benign mandibular tumors or composite defects due to various etiologies mentioned below.
Etiology
Mandibular defects results from surgical excision of:
- Benign mandibular tumors
- Oromandibular malignancy
or, due to:
- Trauma
- Osteoradionecrosis of the mandible.
- Gunshot defects
Classification of Mandibular defects
Several attempts at classifying mandibular defects in a simple and practical way, to aid management, have been made as mentioned below and they have gradually reformed with time as the management for these defects have evolved. Of these, the one put forward by Boyd et al. is the most commonly known system and the one by Schultz et al. is the latest:
- Pavlov- 1974.
- David et al. – 1988.
- Jewer, Boyd et al. (HCL classification)1– 1989, modified by Boyd et al. in 1993.2
- Urken et al. (CRBS classification)- 1991.3
- Schultz et al. – 2015.4
Pavlov classification (1974)
The first attempt at classifying mandibular defects was made by Pavlov (Russia) in the pre-free tissue transfer era.
- Divided mandibular defects into 3 classes based on whether the remaining arch was left in 1, 2 or 3 fragments. (So, class 1 always involved a condyle and class 3 had 2 separate defects)
- Subdivided into groups based on encroachment onto the mentum.
- Further, split into subgroups based on the size of the defect.
- Recognized the reconstructive and functional problem posed by absence of two key element- condyle (reconstructing a condyle is difficult and leads to functional impairment also) and mentum (degloving of chin or resection of entire submental musculature or mentum leads to ptosis of lower lip and chin– ‘Witch’s chin’ / ‘Andy Gump deformity’).
- 16 possibilities of bony defects described.
- Soft tissue defects not considered.
David et al. classification (1988)
- Similar in spirit to HCL classification which was published shortly afterward in 1989 (described below).
- Took into account many reconstructive difficulties mainly related to the resection of the condyle and the central segment.
- Disadvantage- some bony defects (like short H, HCH, HCL, and HC of HCL classification) remained unclassified, soft tissue defects were not classified.
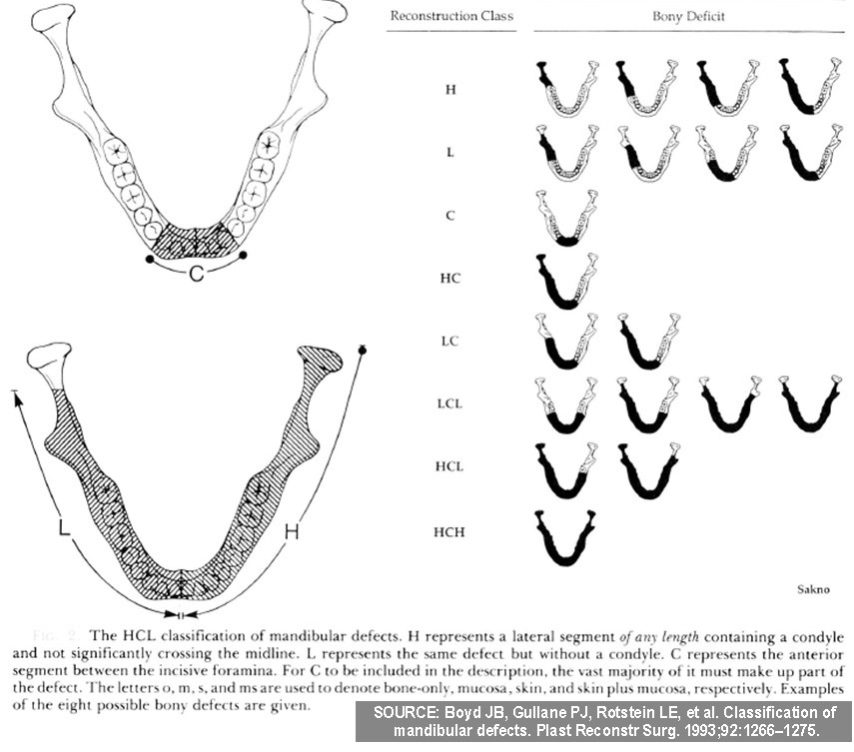
HCL classification by Jewer and Boyd et al. (1989)- modified by Boyd et al. (1993)
This is the most popular classification and still in use for reconstruction of mandibular defects in the free- vascularized free flap era.
- HCL classification is primarily based on reconstructive difficulty.
- It simplified the Pavlov’s classification- as in free tissue transfer era, with the availability of long segments of vascularized bone grafts, the length of the defects lost its significance (non-vascularized bone grafts could be used for a defect size less than 6 cms only)
- So, length of the defect was not taken into account.
- When first published in 1989, it used 3 UPPER case alphabets (H, C, L) to classify bony mandibular defects only, where-
- ‘H’ – (Hemi-mandibulectomy) stands for lateral segment defect ‘of any length’ including the condyle,
- ‘C’ – stands for Central defects including the ‘entire’ anterior segment (including 2 canines and 4 incisors) and,
- ‘L’ – stands for Lateral defects excluding the condyle.
- So, 8 classes of bony defects are possible by the combination of the three alphabets (H, L, C, HC, LC, LCL, HCL/LCH, HCH)
- Note: H and L defects may reach midline and even extend slightly beyond it but unless the entire anterior segment is involved, it’s not classified as HC or LC.
After Urken et al. classified mandibular defects in 1991 (CRBS system- described below) based on soft tissue and nerve defects in addition to bony defect, Boyd modified the HCL classification to include soft tissue component into it in 1993.
- Boyd’s modified HCL classification included soft tissue defects by adding 3 lower case alphabets (o, m, s) as subscripts to the 3 uppercase alphabets (H, C, L) while classifying:
- ‘o’ – no mucosal or skin component,
- ‘m’ – mucosal component,
- ‘s’ – skin component
(So, a subscript of sm indicates both mucosal and skin component.)
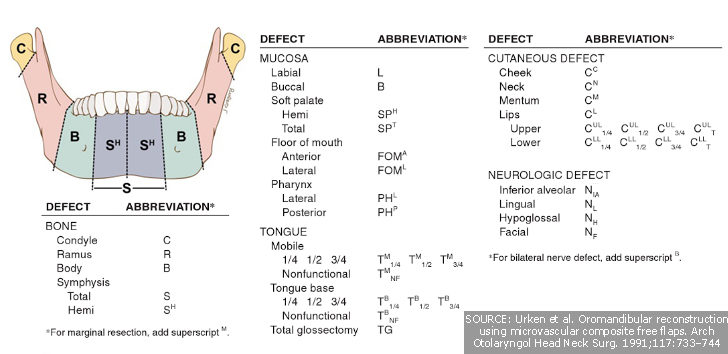
Urken et al. CRBS classification (1991)
Its a comprehensive classification of composite oromandibular defects which includes ‘neurological deficits’ (8 possibilities) in addition to bony (20 possibilities) and soft tissue defects (22 possibilities).
- Bone defects- Condyle, Ramus, Body, Symphysis (S-total, SH: superscript-H indicates- hemisymphysis defect), superscript M to C/R/B/C- indicates marginal resection in that specific part of the mandible.
- Soft tissue defects-
- Mucosa: L- labial, B– Buccal, SP– Soft Palate, FOM– Floor of Mouth;
- T- Tongue,
- C- Cutaneous. The above is again subdivided with various superscripts based on the location of the defect (for eg. anterior, posterior, lateral) in each structure.
- Neurologic defects- N followed by subscript– IA– Inferior Alveolar, L– Lingual, H– Hypoglossal or F– Facial (with a superscript- B for Bilateral involvement).
- Though there are 3500 possibilities and if only bony and soft tissue defects are considered, there would still be 400 possibilities, the nomenclature for bony defects (CRBS) is quite handy to describe the location of disease.
- Highlighted that factors other than size and location of the bony defect also affects the functional and aesthetic outcome of reconstruction.
- Inspired Boyd et al. to modify HCL system to include ‘soft tissue defects’.
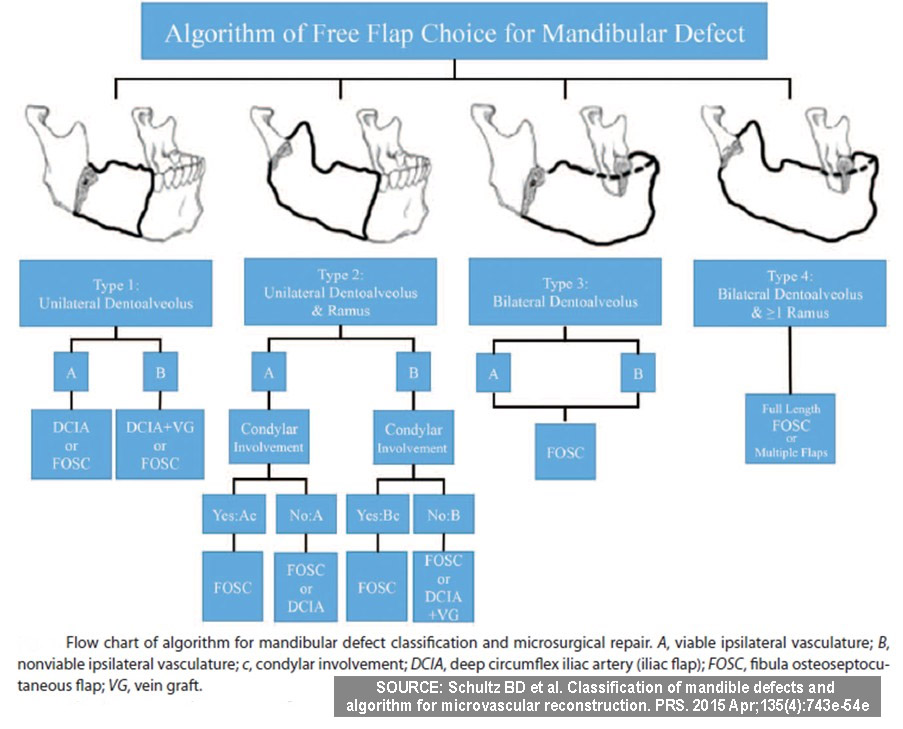
Schultz et al. classification (2015)
It’s an attempt to simplify mandibular defects classification with a focus on the functional mandibular subunits lost and the 2 donor sites for free flaps commonly used for such reconstruction in 2015- Fibular osseoseptocutaneous (FOSC) flap and iliac crest osseocutaneous / DCIA (deep circumflex iliac artery) flap.
- The choice of flap among depends on recipient vasculature (pedicle length requirement) and donor free flap characteristics.
- divided into 4 classes based on ascending order of reconstructive complexity (i.e subunits involved) as shown in the diagram below.
- It’s further divided into ‘A’ and ‘B’ based on the presence or absence of ipsilateral donor vessels.
- ‘c’ when added represents condylar involvement.
- It provides an algorithm for microvascular reconstruction.
As the microsurgical management options of these complex mandibular defects refine further, the detailed sub-classes of the abovementioned classifications may gradually phase off and simplify further for practical purposes.
If you found this post useful subscribe below for more such articles & subscribe to our YouTube channel for video tutorials. You can also find us on Facebook, Twitter and Instagram.
References (For further reading):
- Jewer D D, Boyd J B, Manktelow R T, et al. Orofacial and mandibular reconstruction with the iliac crest free flap: a review of 60 cases and a new method of classification. Plast Reconstr Surg. 1989;84:391–403. discussion 404–405.
- Boyd JB, Gullane PJ, Rotstein LE, et al. Classification of mandibular defects. Plast Reconstr Surg. 1993;92:1266–1275.
- Urken ML, Weinberg H, Vickery C, et al. Oromandibular reconstruction using microvascular composite free flaps. Arch Otolaryngol Head Neck Surg. 1991;117:733–744.
- Schultz BD et al. Classification of mandible defects and algorithm for microvascular reconstruction. Plast Reconstr Surg. 2015 Apr;135(4):743e-54e

Tutorials & tips in Plastic Surgery
+ Weekly updates of high-quality webinars!




How are you, Dr Dev? I found the content to be extremely informative. I’d like to read the articles to assist me in preparing my thesis, but I was unable to access the first three cited. Assuming you have access to them, I’d like to kindly ask that you send them to me via email. Thanks!
Highly appreciated your beautiful way of giving knowledge.